The World Health Organization claims that household air pollution (HAP) kills 4.3 million people per year. Is this true?
Reader Note: This is a work in progress. It is a pretty big job. I will try to add to it regularly and produce a summary report in the end. But I don’t want to just sit on the results as parts are completed. When updates are made, a notice will be posted on JunkScience.
JunkScience.com has already debunked the notion that airborne fine particulate matter (PM2.5) kills either on a short-term or long-term basis. That debunking also applies to HAP. But if you need more evidence specifically on HAP, read on.
This is the 2016 WHO report that makes the claim at issue, “Burning Opportunity: Clean Household Energy for Health, Sustainable Development, and Wellbeing of Women and Children.
The WHO’s claimed “key facts” are:
- Around 3 billion people cook and heat their homes using open fires and simple stoves burning biomass (wood, animal dung and crop waste) and coal.
- Over 4 million people die prematurely from illness attributable to the household air pollution from cooking with solid fuels.
- More than 50% of premature deaths due to pneumonia among children under 5 are caused by the particulate matter (soot) inhaled from household air pollution.
- 3.8 million premature deaths annually from noncommunicable diseases including stroke, ischaemic heart disease, chronic obstructive pulmonary disease (COPD) and lung cancer are attributed to exposure to household air pollution.
Let’s first look at the WHO’s own references purporting to lend credibility to its claims about HAP and death. These references are listed on pages 110-113 of the WHO report.
Study #1. Armstrong JR, Campbell H. Indoor air pollution exposure and lower respiratory infections in young Gambian children. Int J Epidemiol. 1991 Jun;20(2):424-9.
Evaluation. I have marked up the study here. The study does not address death, just respiratory infections — which in any event are not the “noncommunicable diseases” that make up 95% of the WHO’s claim. Exposure to cooking smoke is conflated with exposure to parental smoking. The flaky statistical results are inconsistent between boys and girls. All data is self-reported. There are no measured or even estimated exposures to cooking smoke. This study does not support the WHO claim that cooking smoke causes death.
Study #2. Bates MN et al. Acute lower respiratory infection in childhood and household fuel use in Bhaktapur, Nepal. Environ Health Perspect. 2013 May;121(5):637-42. doi: 10.1289/ehp.1205491. Epub 2013 Mar 1
Evaluation. I have marked up the study here. The study does not address death from noncommunicable disease, merely acute lower respiratory infections. The study is notable for its nonsensical results reporting kerosene was a greater risk factor for illness than biomass burning.
Study #3. Bruce NG et al. Control of household air pollution for child survival: estimates for intervention impacts. BMC Public Health. 2013;13 Suppl 3:S8. doi: 10.1186/1471-2458-13-S3-S8. Epub 2013 Sep 17.
Evaluation. I have marked up this study, here. The child survival estimates are based on results from five studies on indoor smoke and child mortality. The results are all weak associations, mostly not statistically significant. The combination of these studies into a meta-analysis is inappropriate — and still only produces a weak association. Importantly, the results are based on all-cause mortality, an overly broad health endpoint. If indoor air kills, it would logically cause death from heart- and/or lung-related causes. If deaths were limited to just those heart- and/or lung-related, the associations would be even weaker if not nonexistent. We will evaluate the component studies individually later.
Study #4. Chafe Za et al. Household Cooking with Solid Fuels Contributes to Ambient PM2.5 Air Pollution and the Burden of Disease. Environ Health Perspect. 2014 Dec; 122(12): 1314–1320. Published online 2014 Sep 5. doi: 10.1289/ehp.1206340.
Evaluation. This paper merely assumes that fine particulate matter (PM2.5) causes death. It provides no information on whether HAP cause death. It just assumes it does.
Study #5. Chen Y et al. Evidence on the impact of sustained exposure to air pollution on life expectancy from China’s Huai River policy. Proc Natl Acad Sci U S A. 2013 Aug 6;110(32):12936-41. doi: 10.1073/pnas.1300018110. Epub 2013 Jul 8.
Evaluation. This study addresses outdoor air pollution, not HAP. Even so, it does not credibly link particulate matter in outdoor air with death because of its methodological limitations (i.e., it is ecologic epidemiology).
Study #6. Guttikunda SK et al. Particulate pollution in Ulaanbaatar, Mongolia. Air Quality, Atmosphere & Health September 2013, Volume 6, Issue 3, pp 589-601
Evaluation. The study abstract is here. The paper uses models to estimate deaths caused by PM2.5 in outdoor air. The authors assume (vs. try to show) that PM2.5 kills. This assumption is faulty. The study sheds no light on any the key issue deaths from HAP.
Study #7. Janssen N et al. Black Carbon as an Additional Indicator of the Adverse Health Effects of Airborne Particles Compared with PM10 and PM2.5.
Evaluation. The study address vehicle exhaust. It has nothing to do with HAP.
Study #8. Lam NL et al. Kerosene: a review of household uses and their hazards in low- and middle-income countries. J Toxicol Environ Health B Crit Rev. 2012;15(6):396-432. doi: 10.1080/10937404.2012.710134.
Evaluation. This article is a review of other published literature, including the parroting of EPA-funded claims that PM2.5 kills. It contains no original research or data.
Study #9. Lim SS et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec 15; 380(9859): 2224–2260. doi: 10.1016/S0140-6736(12)61766-8.
Evaluation.This is part of the so-called Global Burden of Disease study from which the WHO derives the body count attributable to HAP. This study, however, merely assumes that PM2.5 kills. Thew assumption is based on EPA-funded junk science concerning outdoor air pollution that we have already debunked elsewhere. So it’s not helpful in the determination of whether HAP actually does kill. It is worth observing the following: the notion that one can take the results of epidemiologic studies, throw in some imaginary exposure data across the global population and then calculate global body counts is entirely inappropriate and bankrupt. Epidemiology studies are intended to help determine whether a causal relationship exists, not how large risk may be if a causal relationship is found. This study is statistical malpractice, not science.
Study #10. Smith KR et al. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet Volume 378, No. 9804, p1717–1726, 12 November 2011.
Evaluation. This study reports that reducing indoor wood smoke emissions had no effect on clinically-diagnosed pneumonia in children. This study does not support the WHO’s claims for HAP killing people.
So the above-summarized 10 studies are the published research the WHO cites to support its claims that HAP kills millions per year. In fact, none of these studies support the WHO’s claims on any sort of empirical basis. Now we will turn to examining studies referenced, to the extent this has been done, by the 10 studies — e.g., the component studies of the meta-analysis of Study #3 (Bruce NG) and the studies cited in Study #9 (Global Burden of Disease study).
Study #11. Kashima S et al. Effects of traffic-related outdoor air pollution on respiratory illness and mortality in children, taking into account indoor air pollution, in Indonesia. J Occup Environ Med. 2010 Mar;52(3):340-5. doi: 10.1097/JOM.0b013e3181d44e3f.
Evalulation. This study is included in the meta-analysis by Bruce. Moving past the important fact that the study was designed to study the effects of traffic-related outdoor air quality (not the effects of HAP), the study results, as presented by Bruce, were statistically nonsignificant (i.e., the relative risk confidence intervals all included the no-effect level of 1.0). So this study does not help the WHO’s case.
Study #12. Tielsch JM et al. Exposure to indoor biomass fuel and tobacco smoke and risk of adverse reproductive outcomes, mortality, respiratory morbidity and growth among newborn infants in south India. Int J Epidemiol. 2009 Oct;38(5):1351-63. doi: 10.1093/ije/dyp286. Epub 2009 Sep 16.
Evaluation. This study is included in the meta-analysis by Bruce. The study results are statistically nonsignificant (i.e., the relative risk confidence intervals all included the no-effect level of 1.0). So this study does not help the WHO’s case.
Study #13. Bassani DG et al. Child mortality from solid-fuel use in India: a nationally-representative case-control study. BMC Public Health. 2010; 10: 491. Published online 2010 Aug 17. doi: 10.1186/1471-2458-10-491.
Evaluation. This study is included in the meta-analysis by Bruce. Though the study reports significant associations between indoor solid fuel use and child mortality, the statistical results are weak (i.e., prevalence ratios below 2.0). The insurmountable problem with this study is that all-cause mortality is the health endpoint versus more biologically plausible heart- and lung-related deaths. Limiting the study to biologically plausible deaths would likely dramatically change the results. The authors acknowledge this as follows: “One of the major limitations of the study is the fact that we did not have information on cause-specific mortality in this study.” So this study does not establish that HAPs kill children.
Study #14. Mtango FD. Risk factors for deaths in children under 5 years old in Bagamoyo district, Tanzania.Trop Med Parasitol. 1992 Dec;43(4):229-33.
A copy of this study is not readily available online. The abstract is here. Although the reports a weak association between “child sleeping in the room where cooking is done” and death (relative risk = 2.78), the study was designed to look at risk factors for death and not specifically designed to study the hypothesis that HAP causes death. This poor design also produced an association between “the child eating with others ” and death that was more than three times larger than that for “child sleeping int the room where the cooking is done.” More importantly, the study only considers all-cause mortality, rather than heart- and/or lung-related mortality.
Study #15. Wichmann JL. Influence of cooking and heating fuel use on 1-59 month old mortality in South Africa. Matern Child Health J. 2006 Nov;10(6):553-61.
The abstract for the study is here. The statistical association is weak (relative risk = 1.95) and the confidence interval verges on the no-effect level (1.04 – 3.68). Since the study relies on the all-cause mortality endpoint, these marginal results would likely evaporate if the health endpoint was narrowed to mortality from heart- or lung-related causes. The authors acknowledge “the potential for residual confounding despite adjustment.” Moreover, the study relies on outdoor air pollution junk science to bolster its reported correlation (“the better documented evidence on outdoor air pollution and mortality suggest this association may be real”). But outdoor kills no one and so this study establishes nothing.
So the component studies of the Bruce meta-analysis fail to support the WHO’s claim about HAPs. What about the studies referenced by Study #9, the Global Burden of Disease Study? The study is here. We will be considering these references from Study #9:
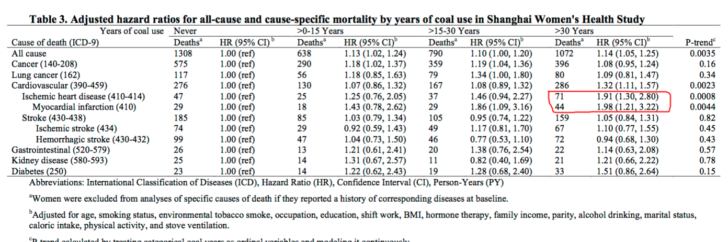
GBOD Referenced Study #132.Pope CA 3rd. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure-response relationships. Environ Health Perspect. 2011 Nov;119(11):1616-21. doi: 10.1289/ehp.1103639. Epub 2011 Jul 19.
Evaluation. This study does not address HAP. The study is an effort by EPA-funded researchers to explain a paradox they created: Low levels of PM2.5 in outdoor cause cause death but much higher levels of PM2.5 from secondhand smoke and direct smoking do not. See GBOD Referenced Study #133, below, for further discussion.
GBOD Referenced Study #133. Pope CA 3rd et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation. 2009 Sep 15;120(11):941-8. doi: 10.1161/CIRCULATIONAHA.109.857888. Epub 2009 Aug 31.
Evaluation. The study does not address HAP. The study is an effort by EPA-funded researchers to explain a paradox they created: Low levels of PM2.5 in outdoor cause cause death but much higher levels of PM2.5 from secondhand smoke and direct smoking do not. Their crazy explanation is that, “The exposure-response relationship between cardiovascular disease mortality and fine particulate matter is relatively steep at low levels of exposure and flattens out at higher exposures.” This phenomenon, of course, directly contradicts the time-honored toxicological principle of “the dose makes the poison.” To do reach this conclusion, basic principles of epidemiology were entirely and wantonly ignored in this paper. The study authors, for example, treated relative risks (i.e, correlations) as probabilistic estimates. This is fundamental malpractice as a relative risk is mere indicator of the strength of correlation in a particular study population; it is not portable measure of risk that may be applied to other populations.
GBOD Referenced Study #134. Krewski D et al. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst. 2009 May;(140):5-114; discussion 115-36.
Evaluation. This study does not address HAP. It addresses PM2.5 in U.S. outdoor air. You can read the synopsis of the study here. But it is irrelevant to the issue at hand — whether and to what extent HAP kills.
GBOD Referenced Study #135. Brook RD et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010 Jun 1;121(21):2331-78. doi: 10.1161/CIR.0b013e3181dbece1. Epub 2010 May 10.
Evaluation. This is not a study of HAP. It purports to be a review of PM2.5 research. It is authored by the usual cabal of EPA-funded researchers. No more need for discussion of it here.
GBOD Referenced Study #136. Committee on the Medical Effects of Air Pollutants. The Mortality Effects of Long-Term Exposure to Particulate Air Pollution in the United Kingdom. London. Health Protection Agency. 2009.
This report is here. It does not address HAP. It merely assumes that PM2.5 in outdoor air kills and then estimates population body counts and years of life lost.
GBOD Referenced Study #137. Cooke RM et al. A probabilistic characterization of the relationship between fine particulate matter and mortality: elicitation of European experts. Environ Sci Technol. 2007 Sep 15;41(18):6598-605.
Evaluation. This study addresses particulate matter from the Kuwait Oil Fires — not HAP. This study suggests that the risk of death from PM2.5 may be greater than estimated by other outdoor air studies — which not only is not justified by any facts but directly contradicts the GBOD studies authored by Pope mentioned above.
GBOD Referenced Study #138. Burnett RT et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect. 2014 Apr;122(4):397-403. doi: 10.1289/ehp.1307049. Epub 2014 Feb 11.
Evaluation. The study is here. It does not address the key issue of whether HAP causes death; it merely assumes that it does.
GBOD Referenced Study #139. Baumgartner J et al. Indoor air pollution and blood pressure in adult women living in rural China. GBOD Referenced Study #138.
Evaluation. The study reports that HAP “may” be associated with slight increases in blood pressure. Not only are the estimated increases slight, clinically insignificant and of speculative long-term health impact, they are not death. So this study does not support the WHO’s claim of HAP causing death.
GBOD Referenced Study #140. Smith KR et al. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet Volume 378, No. 9804, p1717–1726, 12 November 2011.
Evaluation. This study has already been evaluated (Study #10, above) as unhelpful to the WHO.s HAP claim.
We will now examine other published studies on HAP to see if any support the WHO’s claims. If you run across a study that is not evaluated here, please feel free to submit it to JunkScience.com.
First, we will evaluate studies found through PubMed with the search term “household air pollution and mortality.”
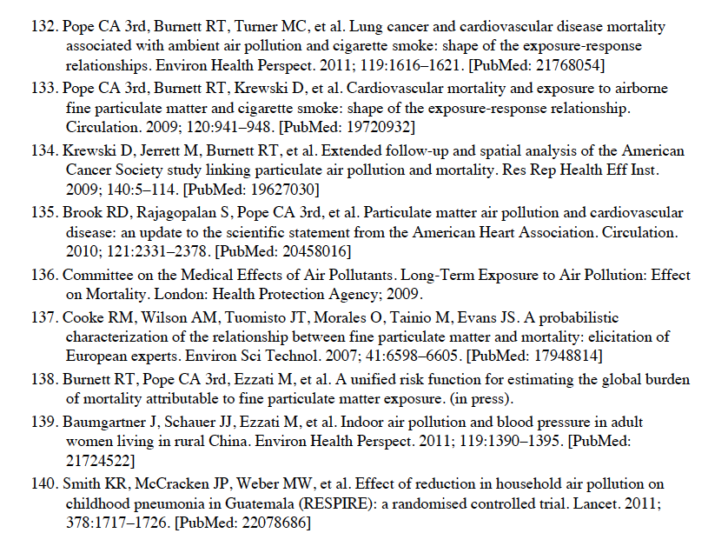
PubMed Study #1. Mitter SS et al. Household Fuel Use and Cardiovascular Disease Mortality: Golestan Cohort Study. Circulation. 2016 Jun 14;133(24):2360-9. doi: 10.1161/CIRCULATIONAHA.115.020288.
Evaluation. The study is here ($$$). The table with the results is below.
As you can see, all the associations are “no effect”, weak and/or statistically insignificant — al of which means this study reports nothing of interest. Though the authors tout the kerosene/diesel results, kerosene and diesel burn cleaner than wood or animal dung. This study does not help WHO’s case that HAP cause death.
PubMed Study #2. Naz S et al. Household air pollution and under-five mortality in India (1992-2006). Environ Health. 2016 Apr 26;15:54. doi: 10.1186/s12940-016-0138-8.
Evaluation. The study is here. More weak statistical associations in a study where the health endpoint was all-cause mortality, which over-includes deaths potentially attributable to HAP. Much study “data” is self-reported and not subject to verification. The authors rely on the WHO’s GBOD study to support their conclusions. But as pointed out earlier, the GBOD study relies on debunked EPA junk science.
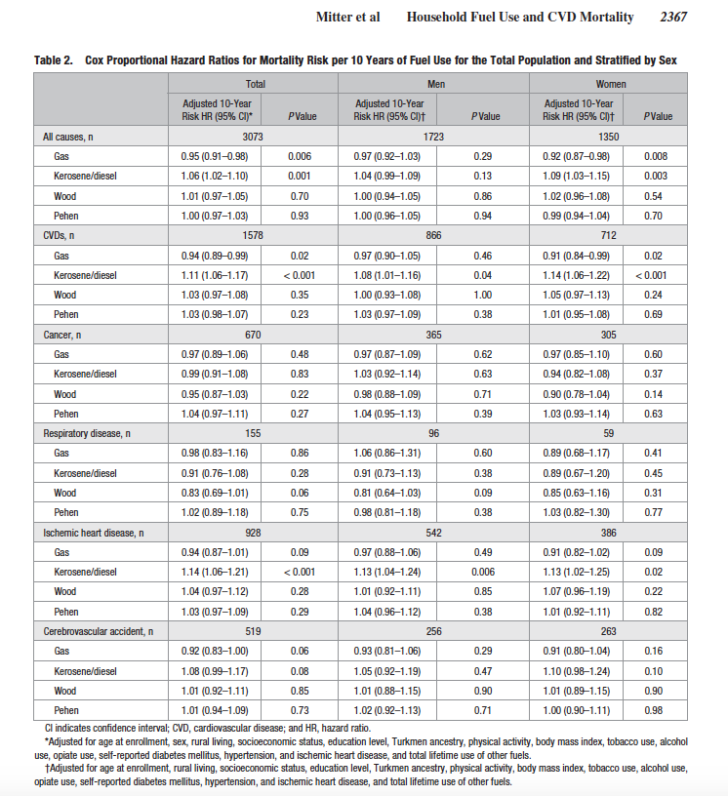
PubMed Study #3. Kim C et al. Cooking Coal Use and All-Cause and Cause-Specific Mortality in a Prospective Cohort Study of Women in Shanghai, China. Environ Health Perspect. 2016 Apr 19.
Evaluation. The study is here. The result of interest is highlighted in the table, below.
While the study is easily dismissed because of its weak and/or nonsignificant associations, for the sake of argument, let’s not do that for the highlighted result. The group of women at issue (coal use for 30+ years) seems to contain somewhere between 10,000 to 15,000 women. Yet only 115 are in the group have supposedly died from heart disease. That is a very small group. Heart disease is very common. The exposures to PM2.5 are not known by the researchers. Not persuasive.
PubMed Study #4. Patel AB et al. Impact of exposure to cooking fuels on stillbirths, perinatal, very early and late neonatal mortality – a multicenter prospective cohort study in rural communities in India, Pakistan, Kenya, Zambia and Guatemala. Matern Health Neonatol Perinatol. 2015 Jul 21;1:18. doi: 10.1186/s40748-015-0019-0. eCollection 2015.
Evaluation. The study is here. Its weak associations are further attenuated/eviscerated by failure determine whether cooking was indoor or outdoor, failure to account for socio-economic status and failure to ascertain medical cause of reported miscarriages. Also note the weak association become nonsignificant in babies that survive the first three days.
Another very dangerous “indoor air pollutant” that is not mentioned is toxic mold.
Bill: I agree.
Nikhil: You use the example as smoke being a risk factor to COPD, but if the actual deaths due to COPD = 0, then the risk factor is irrelevant to attributing deaths (which is what this original post is all about, the WHO attributing millions of actual deaths to something).
I do not disagree with the notion of risk factors, but you can’t use an inflammatory claim like 4 mil deaths. The implication is that if this risk had been removed, those 4 mil would still be alive which is false.
The use of dried animal dung for fuel is ubiquitous and timeless. It is a GOOD thing.
Dino: Your question was about the UN. You seem to know the answer. I don’t need to opine.
To NIKHIL: WHO reported it, therefore they support the BS. My question is valid regardless of the researcher, reporter, or your opinion.
To Dino: This is not WHO. It is merely reporting academic research. Much of it sponsored by USEPA and used in its regulatory justifications, agreed to by the Supreme Court so far. That is the law; the rest is sniping.
To Kuhmkat: I need only repeat – “Correlations matter.” I leave academics to argue causality; they are experts in wasting time.
To Allen Brooks: As far as “cause of death” goes, yes. To repeat, premature mortality or DALY is not an individual attribute. I am shocked at meth reference. Will check out. Thank you.
Perhaps the leading cause of death from indoor air pollution is CO. Radon daughters can also be threat and they are usually closely monitored. But the most subtle and dangerous cause of indoor air pollution is meth. We don’t hear much about it because it is not politically correct to do so. It would expose the extent of the abuse. Only recently a company formed in our city to test and decontaminate meth contaminated housing (meth busters)
Nikhil, thanks for clarifying your useless first post. Now, what is the evidence that COPD or ALRI causes death and is caused or made worse by the particulate?!?!
Is there anything from the United Nations that is true?
Re: Kuhnkat
The question is not whether smoke makes anybody sick. But whether exposure to smoke is a risk factor for ALRI or COPD.
Correlations matter.
Nikhil:
“Smoke is sickening. It doesn’t take even grade school to know that.”
I have been sick many times in my life. I am not dead. Something causing me to be sick is not a strong indication of an actual death or even possibility of a death. Correlation is not causation. Write that a few million times.
I seem to recall
– In Asia many women are dying in their 30’s from cooking over open wood fires indoors.
– In the US some days may be knocked off the end of some people’s live due to traffic particulate pollution.
Any news report that uses raw deaths is junk, cos it is Quality Adjusted Life Days that should be counted.
…cos death comes to 100% of humans (so far)
Re: Andrew Kerber
Yes, that is correct. But it applies to actual disease and deaths. Premature mortality is about apportioning the diseases to risk factors, which may overlap, as is the case with CO and PM.
It would really be interesting to know how many of those deaths of children in the room where cooking occurred were due to CO poisoning, rather than particulates. Clearly in places where ventilation is poor, CO poisoning could be a problem.
Bill wrote: “life expectancy is rising which implies that there would have been MORE premature deaths in the past (sic) when levels were lower. So is 3.8 million deaths (assuming the number is anywhere remotely accurate) a bad thing or is a valid argument that all this PM2.5 actually reduces premature death (and explains the rise in life expectancy) >:)”
You got this partly correct. Yes, life expectancy is rising, for whatever reason. Premature mortality is increasing because the number of deaths are increasing, including before the new life expectancy, because even if later, people have to die.
When there is more premature mortality, and the prevalence of other risk factors or diseases declining, of course more premature mortality is attributed to solid fuel use. (Yes, something has to be blamed.) Read the Kirk Smith paper on how the numbers went from below 1 million to nearly 4 million.
Bill also, “The LE/cause/risk factor methodology, for example, may have predicted things fairly well in the 1950s/60s/70s before mass migrations of populations and globalization became the norm but does that same method reliable now? ”
Premature mortality is NOT a matter of prediction, only history, and only for parceling out numbers. The question is, are dose-response equations of the past applicable today as air has become much cleaner, people on average have a different nutrition and health profiles?
Bill wrote: “life expectancy is rising which implies that there would have been MORE premature deaths in the past (sic) when levels were lower. So is 3.8 million deaths (assuming the number is anywhere remotely accurate) a bad thing or is a valid argument that all this PM2.5 actually reduces premature death (and explains the rise in life expectancy) >:)”
You got this partly correct. Yes, life expectancy is rising, for whatever reason. Premature mortality is increasing because the number of deaths are increasing, including before the new life expectancy, because even if later, people have to die.
When there is more premature mortality, and the prevalence of other risk factors or diseases declining, of course more premature mortality is attributed to solid fuel use. (Yes, something has to be blamed.) Read the Kirk Smith paper on how the numbers went from below 1 million to nearly 4 million.
Bill also, “The LE/cause/risk factor methodology, for example, may have predicted things fairly well in the 1950s/60s/70s before mass migrations of populations and globalization became the norm but does that same method reliable now? ”
Premature mortality is NOT a matter of prediction, only history, and only for parceling out numbers.
@Allen Brooks, perhaps this is the reason why the Government is now focusing so much on PM2.5. With the drives to legalize marijuana this provides an additional avenue for them to regulate and provide kickbacks to winners? Perhaps there is a company already developing a method of measuring PM2.5 like a calorie count and it’s a way to make money through labeling requirements. /sarcasm off. Of course, it will likely just be a completely made up number like the fuel economy ratings on the new car window sticker.
Well, the other thing you have to consider with the statistical work is that the don’t know what side they are on. 3.8 million premature deaths, but life expectancy is rising which implies that there would have been MORE premature deaths in the past when levels were lower. So is 3.8 million deaths (assuming the number is anywhere remotely accurate) a bad thing or is a valid argument that all this PM2.5 actually reduces premature death (and explains the rise in life expectancy) >:)
FYI, for perspective, i’m a computer scientist who works in large data set analytics and business intelligence…now “sold” as “Big Data” by the vendors selling tools and trying to reinvent the field because data warehousing got a bad name as a money sink to the same vendors. The naive often overlook questioning the validity of a dataset simply because a prior set of results fit the real worldand therefore any further questioning is avoided — ignoring that the dataset is evolving and not static. The LE/cause/risk factor methodology, for example, may have predicted things fairly well in the 1950s/60s/70s before mass migrations of populations and globalization became the norm but does that same method reliable now? We have the same discussions regarding economic policies but focusing on medicine: the WHO puts out “grades” of country medical systems and included in there is infant mortality which is one of the elements the policy makers pull out to lambast how bad the US medical system is. However, one could argue that infant mortality in the US is artificially high and in other countries artificially low simply due to migration. Just recently we had a South American woman with Zika who’s ultrasound showed that her fetus was defective. She traveled to the US where the baby was delivered and now being cared for in New Jersey. Should this child not survive they become part of the US statistic and not the statistic of their native country. The statistic used to demonstrate how poor the US system is actually demonstrates the inverse once the dataset is evaluated and not simply analyzed using statistical and meta analysis.
Hopefully this illustrates why I am very skeptical of any calculated “deaths.”
I wrote “EPA assumes too many things in its computations.”
But who am I to judge? EPA says scientific assessment of literature and review of the assessment by its advisory body underlie its assumptions. I haven’t checked. If the Supreme Court grants the Chevron deference, it doesn’t matter what others say. Or think.
Allen Brooks: That precisely is the point. There are NO autopsy reports listing “indoor air pollution” as the cause of death.
Actual deaths have causes. The aggregate of premature mortality is computed and statistically allocated to “risk factors”.
In a recent Lancet paper, “risk factors” for premature mortality among the youth (10-24) included unsafe water, alcohol use, drug use, handwashing, unsafe sex, high blood pressure and yes, household air pollution.
These are “risk factors” that contribute to incidence of diseases that lead to premature deaths. Conversely, premature mortality is not caused by these risk factors but can be appoprtioned among these risk factors or can be said to be attributable to these risk factors.
The methods, data, and interpretations require many assumptions. In any case, premature mortality attributable to household air pollution varies over time, not the least because incidence of other diseases (than those where household air pollution is a risk factor) may change, their treatment improves, or that nutrition and exercise profile changes.
EPA assumes too many things in its computations.
nikhil: If “it has nothing to do with specific deaths” how can it be linked to “indoor air pollution? Where are the autopsy reports listing “indoor air pollution” as the cause of death? And yes tobacco smoke is sickening, but the same crowd that shouts this has no problem with pot, which is far worse.
Paper on China at http://www.pnas.org/content/early/2016/06/21/1604537113.
A press release at http://phys.org/news/2016-06-household-fuels-major-contributor-beijing.html.
My commentary:
Kirk Smith and colleagues: “We show that due to uncontrolled and inefficient combustion of solid fuels in household devices, emission reductions from the residential sector may have greater air quality benefits in the North China Plain, including Beijing, than reductions from other sectors.”
“Reduction of emissions from the residential sector via the replacement of solid fuels with other cleaner energy sources could substantially improve air quality in the BTH region of eastern China.”
Amen. Substituting grid power (high share of coal) and electric cooking (rice cooker to kettle to stovetop and ovens) and heating for the next 25 years (while gas and renewables come up) would be good for the children of Mother Earth, even if not for the Mother. (And which mother would mind that?)
Oh, wait a minute. Aerosols from coal power largely negate the radiative forcing due to their CO2. So coal power is cleaner both for health as well as climate.
All emissions and all impacts considered – and discounted for time, uncertainty, and expert biases, modern energy transition for the poor is beneficial to them, their governments, and the planet.
But some children of mother earth don’t care about their siblings.
This is in response to Bill who wrote about causes of death as reported on death certificates (DC).
I wish the cooking up of risk factor allocations of premature mortality were that simple.
Premature mortality is a population metric, not individual metric. Bill’s father’s premature death was from multiple “causes” but “causes” at individual level do not come into play. For every “population”, there are reported “causes”, as in the case of Bill’s father. But not all deaths are premature (roughly only a half), and life expectancies and premature mortality are specific only for a particular year.
Say, the total male deaths in US in 2000 were 1.2 million, and life expectancy for males was 75 for that cohort (changes very slowly). Say, only 500,000 were before 75.
Then there is a distribution from reported causes of death. (These have weaknesses, more so in poorer areas of the world. Lancet had an excellent, searing piece a year or two ago.) All the causes are aggregated, then distributed to “risk factors” – say, 100,000 due to CHF are given x% to obesity, y% to smoking, z% to something, etc. This allocation uses statistical methods and heroic assumptions in part based on specific epidemiological studies but very loosely; studies are not that consistent and the populations are not comparable. In any case, deaths any particular year have an unknown distribution of “confounding factors” – nutritional history, genetics – that is different from deaths for any other populations. Mislabeling of causes of individual deaths makes little difference.
Why is this exercise done every few years, considering all the qualifiers that must be attached? To get an idea of “disease control priorities”.
Thus, for instance, a recent paper in PNAS (I will post later) argued that in North China, air quality improvements from interventions in the residential sector are more promising than in other sectors. I think it is an important statement, even with qualifiers for exact numbers. It says, as VicB3 recommends above, that a coal power plant can help clean up the air from residential uncontrolled use of unprocessed solid fuels.
To Milloy re: his opening note – Armstrong (1991) had ALRI as a more prominent cause because i) it is a cause, not a risk factor, and ii) it is for a year with a different distribution of deaths and life expectancies (and also when air pollution may ave been lower.) Read a paper on Kirk R. Smith website about how premature mortality allocation to Household Air Pollution shot up from 1 million to 4 million. It will also help understand the method behind the madness.
Sorry, I don’t mean this to come off sarcastic but I find it funny people think that the entries on the death certificate are accurate. My father had a heart attack and died. The DC said the cause was CHF; however, he had a previously diagnosed heart defect (diagnosed 20+ years prior). Now, he had fluid on his lungs, so everyone assumed CHF but the autopsy said the fluid was not consistent with CHF but instead consistent with infection. So now, we have a man who had a heart defect who had a lung infection which resulted in a heart attack. Death cert is heart attack, my doctors are all now trying to prescribe mega doses of every cardiac drug known to man because of my father’s death when the reality is he caught some sort of lung infection, went for 3+ months before getting it checked out. That 3 month long “walking pneumonia” then causes his heart to work harder causing it to swell (same as CHF) and when the defect was interjected — death.
My point? What was the cause of his premature death? Was it even premature since he had a genetic heart defect? I’m sure he is included in the PM2.5 deaths somewhere simply because he had a heart attack so it must have been caused by PM2.5, not possibly an infection where the patient didn’t seek treatment until the damage had been done. The lung infection be damned (there was even early speculation of lung cancer but he passed before those tests had been conducted — his physician was shotgunning ideas of what was causing the fluid since it wasn’t responding to antibiotics or digitalis).
Analysis conducted from death certificate causes is flawed IMO.
Allen Brooks says, “If there is any form of “indoor air pollution” and someone dies, (regardless of the cause, even automobile accidents or murder) they will use the numbers to prove their case.”
This is simply not true. Premature mortality is a population concept, and isk factors a matter of allocating these deaths. It has nothing to do with specific deaths.
Smoke is sickening. It doesn’t take even grade school to know that.
1 – Indoor pollution isn’t the problem (if indeed it is), it’s the lack of ventilation. Tell somebody to open the damned window.
2 – Build a few power plants and install some natural gas lines, add some modern appliances, and the problem will go away. In other words, let loose the market driven economy and the problem will solve itself quickly as people acquire wealth. Except for the odd outdoor BBQ, camping trip or romantic evening, nobody willingly burns wood or lights candles for cooking, lighting, heating or whatever if they don’t have to.
Just a thought.
VicB3
If there is any form of “indoor air pollution” and someone dies, (regardless of the cause, even automobile accidents or murder) they will use the numbers to prove their case.
If indoor air pollution was deadly, humanity would have been practically made extinct due to smoke from open fires in caves.
Stan B gets it right – “We have to blame something.” Grants are needed and authorized, but the whole question of “risk factors” is, what is important and ow much, so we can prioritize various options for better health?
Science helps only in setting priorities. But priorities cannot be set in isolation. The air pollution community obsesses over PM2.5 and the unknown dose-response relationships to allocate the burden of disease, while ignoring the most dangerous air pollutants among the PM2.5! Air quality monitors do not measure all PM2.5 at all levels. Walk around any poor area in Asia or Africa and you’d see fires, chemical spills, open waste, and noxious gases, close to the ground level. This pollution is not measured.
Spurious data, unsupported assumptions, unvalidated models. An open marriage of regulators, advocacy groups, and academia.
Has anybody but me noticed that longevity has become a commercially-motivated “competition?” Apparently, he who lives the longest, sucking up the most disease-care dollars, “wins.” Otherwise, why the ongoing obsession with the “risk factors” of everyone else’s “health?” Most of American “primary care” no longer is treating actual DISEASE–it is treating statistical constructs of dubious merit at enormous expense and misery to individuals. Why play the game? Anything coming out of the WHO is already suspect given their ridiculously unattainable definition of “wellness.”
We have to blame something, or the grant money dries up!
Exposure to air pollution in general – and to air pollution from solid fuel use in household cooking and heating – is a “risk factor” in the diseases – COPD and other – that are in turn implicated in actual deaths. Risk factors do not cause a disease or a death. Premature deaths are not individual deaths. They are a construct – deaths before a life expectancy appropriate to a particular population (in itself a debatable construct *), which changes with every 10-year cohort – and the total of those premature deaths are allocated, via the use of debatable methods and assumptions, to different “risk factors”. (Nobody bothers about the post-mature mortality, which has almost as many people though fewer years; arguably, the “risk factors” for premature mortality should be netted out against their contribution to post-mature mortality – e.g., by the number of years cigarette smokers die BEYOND life expectancy.)
The question is not whether 4 million premature deaths are allocated to household solid fuel pollutants but rather, if not, which risk factors should they be ascribed to?
WHO statements that you cite should be corrected as “premature deaths attributed to”, leaving aside the issue of whether the methods of attribution are valid. The assumption is, if experts agree that methods are valid, then the numbers are valid for experts; others don’t have to agree with experts. (Group consensus has its advantages and disadvantages.)
So,
Over 4 million premature deaths are from illness attributed to.. These include “More than 50% of premature deaths due to pneumonia among children under 5 ..” and “3.8 million premature deaths annually from noncommunicable diseases”
That is, from the total number of premature deaths from non-communicable diseases such as “stroke, ischaemic heart disease, chronic obstructive pulmonary disease (COPD) and lung cancer”, 3.8 million “are attributed to exposure to household air pollution.”
I am not sure an individual actually dies from just one of these particular diseases, though only one cause may be listed for cause. (I suspect more than a half of the deaths now still do not have a validated cause of death. Not many deaths occur in hospitals and death certificates are iffy.) Each death may have multiple illnesses and each illness may have multiple risk factors.
Attribution is an allocation game. No claim is made for biological causality. Allocation in turn comes from
* I am an Indian immigrant to the US. Which life expectancy should my death be compared to? Indian males of 1950s or 2030s? American males of those 2010s?
This reminds me of the argument over the health effects of marijuana.
The pro-pot crowd claims there are no deaths linked to pot use, yet there is no easy way for those filling out death certificates to say that pot use was, or was not a factor without performing tests that cost money and may not be conclusive.
But no one will raise an eyebrow if they check the box for “tobacco”.
If enough people “in the system” accept a premise, it is not easy to refute it.
Let’s pick a number and see if it sticks.